Understanding The Wound Healing Process
From the desk of an Aesthetic and Wound Care Nurse / August 08, 2022
Are you interested in aesthetic treatments? Or perhaps, you are getting microneedle, laser treatments, PRF or PRP facial, and want to make sense of it all. I’m glad you are intrigued to learn about the amazing way our body operates and tries to heal itself. Feel free to come back here should you need a refresher in case you are undergoing a cosmetic procedure and are wondering if your healing is coming along as expected.
What is skin?
Skin is the body’s largest organ covering the entire body and is the first line of defense. The skin serves to protect us from the external elements such as moisture, sun, bacteria, chemicals, and temperatures.
The skin has many functions:
- Regulate body temperature
- Prevent trans-epidermal water loss - TEWL
- Protect from bacteria entry
- Produces vitamin D with exposure to sun
- Serves as skin barrier to physical insults

The Skin is made up of 3 layers:
1. Epidermis - the outermost layer which, itself, is comprised of 5 layers.
A. Stratum corneum - outermost layer, wherein keratinocytes (keratin) become corneocytes. Corneocytes are strong, dead keratinocytes that is eventually shed during process called desquamation. New keratinocyte cells are constantly produced in stratum basale layer and continues to differentiate while moving upwards to the surface pushing the old cells to be desquamated.
B. Stratum lucidum - thin transparent layer of keratinocytes, found only in areas with thick skin such as palms of hands, fingertips, and soles of feet. Think fingerprints.
C. Stratum granulosum - cells accumulate lipid containing granules which along with desmosomes, form waterproof barrier to help prevent fluid loss from skin. This is otherwise known as keratinization.
D. Stratum spinosum - also squamous cell layer. These are maturing basal cells that are now called squamous cells, or keratinocytes. These appear crushed and are held together by sticky proteins called desmosomes like glue. Langerhans cells, are dendritic cells as they have legs, reside in this layer. LC regulate the immune system, in that they determine the appropriate immune response - inflammation vs tolerance. LC are specialized at “sensing” the environment by stretching its dendrites (or legs) to the outermost layer of epidermis to sample foreign substance. LC perform phagocytosis where they swallow the foreign body, transport and present to other immune cells to stimulate immune reaction. LC have the ability for tumor recognition as well as microbes. Sunlight impairs LC, and it is for this reason that adequate SPF is recommended to prevent skin cancer.
E. Stratum basale - also stratum germinativum,is the deepest layer of epidermis separated by the basement membrane from the dermis. Contains keratinocyte stem cells which produce new cells. Also, contains melanocytes which produce melanin - pigment that gives color to epidermis. As basal cells produce new cells, old cells are pushed out to be sloughed off.
Epidermis contains 4 types of cells:
- Keratinocytes - predominant epidermal cell type originating and produced continually in the basal layer. Produces the protein keratin which form hair, nails, the outer skin. The outermost layer, also corneocytes the dead cells, is naturally shed as part of skin cycle is called the stratum cornea.
- Langerhans’ Cells - are skin’s army. Found in stratum spinosum.
- Merkel Cells - found in stratum basale above basement membrane, responsible for light touch.
- Melanocytes - also at base of epidermis, produce melanin which gives color to skin. Has long arms which deposit melanosome containing the pigment melanin to adjacent keratinocytes. **UVB stimulates melanin production as a protective mechanism against UV damage. Melanocytes is essentially functioning as your internal sunscreen. Hence, adequate sunscreen protection is recommended to prevent over-activation of melanocytes. Melanin is produced by conversion of tyrosine to dopa by enzyme called tyrosinase
which is located in melanocytes. Therefore, another approach used to mitigate hyperpigmentation is the use of Tyrosinase Inhibitors such as Kojic Acid, Tranexamic Acid, Alpha Arbutin, L Ascorbic Acid, and Hydroquinone in skincare products.
2. Dermis - the middle layer of the skin where fibroblasts are found. Fibroblasts play an important role in wound healing. They are involved in breaking down fibrin clot, creating
collagen and extracellular matrix (ECM), elastin, and causing wound contraction. Collagen gives skin structure and strength, while elastin (think elastic) gives the skin flexibility. Also contains blood vessels, lymph vessels, hair follicles, sweat glands, collagen bundles, nerves, and sebaceous glands.
3. Subcutaneous fat layer - the deepest layer of the skin consisting of a network of collagen and fat cells. Helps conserve body’s heat, protects body from injury by acting as a shock absorber.
Now that we got this brief anatomy review out of the way, let’s delve right into the body’s natural wound repair process.
What is a wound?
Because skin is our first line of defense against external factors, it is easy to damage it. A wound is created as soon as skin is injured. This happens when there is a break in the skin continuum whether it is from a trauma, infection, or from a pathological process such as inflammation. Upon skin injury, the body’s wound healing process is immediately activated in order to preserve itself and repair.
What is a wound?
Because skin is our first line of defense against external factors, it is easy to damage it. A wound is created as soon as skin is injured. This happens when there is a break in the skin continuum whether it is from a trauma, infection, or from a pathological process such as inflammation. Upon skin injury, the body’s wound healing process is immediately activated in order to preserve itself and repair.
How does a wound heal?
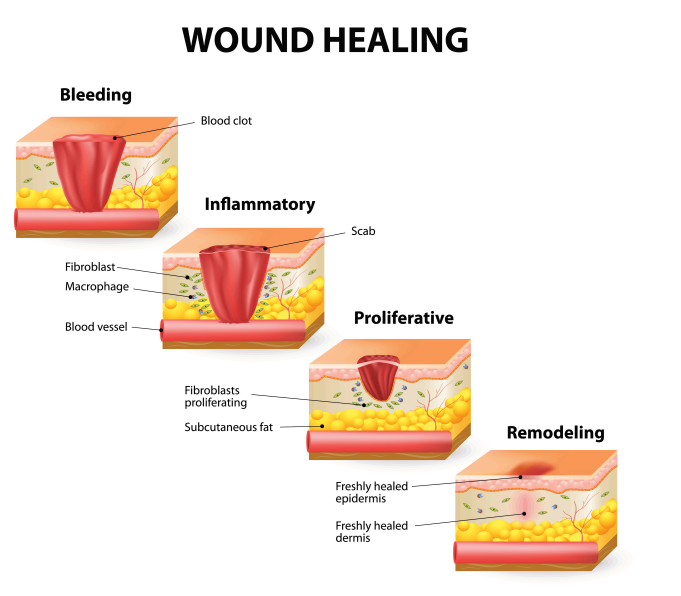
1. Hemostasis - Lasts up to 2 days. When bleeding starts after a skin injury, within seconds or minutes, platelets aggregate to form a fibrin clot to seal off the ruptured blood vessel wall. As name suggests, purpose is to stop further blood loss. This clot will turn into a scab as they dry out over time. **Note: Avoid picking at scabs, this disrupts wound healing, and can cause scarring.
2. Inflammatory Phase - Up to 7 days in acute wounds. This happens when injured blood vessels leak transudate, refers to fluid buildup in tissues causing edema, redness, heat, and pain. White blood cells enter wound, neutrophils destroy bacteria in the early inflammatory phase; in the late inflammatory phase, monocytes mature into macrophages which remove debris, dead neutrophils, and damaged tissue. Macrophages also secrete growth factors, cytokines and chemokines which are signaling molecules part of the immune
response. Cytokines are used by immune cells to communicate with one another, while chemokines guide the migration and localization of immune cells. This phase is the “cleaning up” phase to prepare wound bed for new tissue growth.
3. Proliferation - 4 to 21 days. Wound is rebuilt by fibroblasts with formation of new tissue growth made up with collagen and the extracellular matrix (ECM). Extra-cellular, extra refers to the outside environment of cells. ECM enable cells to attach and communicate with each other. Characterized by formation of granulation tissue, angiogenesis (blood vessel formation), wound contraction (wound closing off from edges), and epithelialization. How long it takes for tissue regeneration depends on collagen production by fibroblasts. **Note: Epithelialization happens faster when wounds are kept moist and hydrated.
4. Remodeling - 21 days to 2 years or longer. Also called Maturation Phase. Collagen production continues to strengthen healing skin. Collagen type III convert to type I in
this stage. Wound continues to contract and fibers reorganized. In phase 3, collagen may be disorganized. In this phase, collagen is reorganized so they lie closer together in a
more organized fashion and cross-link. Cross-linking reduces scar thickness and strengthens wound area. **Of note, healed wound has 80% tensile strength of uninjured skin. tinues to contract and fibers reorganized. In phase 3, collagen may be disorganized. In this phase, collagen is reorganized so they lie closer together in a more organized fashion and cross-link. Cross-linking reduces scar thickness and strengthens wound area. **Of note, healed wound has 80% tensile strength of uninjured skin.

Skincare tips:
• Apply and reapply broad spectrum sunscreen which protects skin from both UVA and UVB. SPF 30 at minimum and reapply every 2 hours. Not only does this help prevent skin cancer, but sunscreen also helps prevent stimulation of melanocytes from producing melanin. Broad spectrum sunscreens offer both UVA and UVB protection coverage.
A. SPF - Sun Protection Factor measures how effective a sunscreen is at protecting skin from UVB rays. SPF 30 give 97% protection.
B. PA ++++ - measures how much protection a sunscreen has from UVA rays. The number of plus (+) symbols signify the protection grade with 4 plus symbols being the highest.
• Add Tyrosinase Inhibitors to your skincare routine to help reduce melanin production. Tyrosinase converts tyrosine to dopa producing the pigment. Therefore, inhibiting the conversion will prevent the production of the pigment melanin.
Examples are Vitamin C, Hydroquinone, Kojic Acid, Tranexamic Acid.
• Hyperpigmentation refers to concentration of pigments in certain areas. This happens commonly with dry skin. When skin is adequately hydrated, melanin is more EVENLY distributed throughout resulting in even skin tone. How do you optimize even distribution is by incorporating humectants such as hyaluronic acid, beta glucan, and glycerin. Humectants draw water to the skin surface and retain them. Then top off with a good moisturizer to prevent TEWL.
• After microneedling, non-ablative laser procedures, or chemical peels, do promote epithelialization by keeping your skin moist and hydrated. Optimize healing with Hyaluronic acid, growth factor serums, moisturizer. Reapplication of these to prevent skin from feeling dry and tight will help. Refer to your aesthetic provider’s instructions.
• The controlled skin trauma caused by microneedling, or other aesthetic procedures, increases skin cell turnover. This refers to the process of producing new skin cells to replace existing skin cells. This may present by skin peeling. Although at times, this may be mild that you can’t visualize the shedding of skin. Skin may feel dry and tight. This is because there is more transepidermal water loss (TEWL) during this time as there is a
breach in the skin.
References
InformedHealth.org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-. How does skin work? 2009 Sep 28 [Updated 2019 Apr 11]
Yousef H, Alhajj M, Sharma S. Anatomy, Skin (Integument), Epidermis. [Updated 2021 Nov 19]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470464/
Wound Source. Wound Healing. Available from:https://www.woundsource.com/blog/four-stages-wound-healing

